CARDIOVASCULAR REVIEW 3: CONTROL of BLOOD PRESSURE, ALL MECHANISMS, Animation
– Blood moves away from the heart in arteries, and back in veins. Blood flows from heart to aorta, to large arteries, then smaller arteries, arterioles, capillaries, then venules, larger veins and back to the heart. – The walls of arteries and veins consist of 3 layers: outer connective tissue, middle smooth muscle, and inner endothelium. Smooth muscle allows blood vessels to constrict or dilate, regulating blood flow. The walls of capillaries consist solely of a thin endothelium to permit easy exchange of substances. – Blood pressure is the force the circulating blood exerts on the walls of blood vessels.
It is highest when blood exits the heart, and decreases as it moves away. – Blood flow is the amount of blood passing through a tissue or vessel in a given time. Perfusion is the flow per given volume or mass of tissue. Flow is directly proportional to the pressure difference between 2 points, and inversely proportional to resistance. Blood flow is highest in the aorta and large arteries, lowest in capillaries, and somewhat higher in veins. – A person’s blood pressure, or systemic arterial pressure, is the pressure measured in larger arteries. It is directly proportional to cardiac output,
blood volume and vascular resistance. Blood pressure is typically regulated by changing heart rate, stroke volume, blood volume, or vessel radius. – Systemic blood pressure is regulated by 2
the ANS, the PSNS, decreases heart rate by releasing acetylcholine which acts to reduce the excitability of the SA node and AV node. PSNS activation results in lower blood pressure. – On the other hand, the sympathetic arm, the SNS, releases norepinephrine which acts on the SA node to increase heart rate; on cardiac myocytes to increase stroke volume, and on vascular smooth muscle to cause vasoconstriction. Thus, SNS activation leads to higher blood pressure. – Most prominent inputs are from baroreceptors, which detect changes in blood pressure. Baroreceptors are stretch receptors located mainly in the wall of the aortic
arch and carotid sinus. Increased blood pressure stretches blood vessel wall, causing baroreceptors to fire action potentials at a higher than normal rate. These activities are sent via the vagus and glossopharyngeal nerves to the solitary nucleus, the NTS, of the cardiovascular center. In response, the center activates the PSNS and inhibits the SNS, bringing blood pressure back down to normal level. The reverse happens when blood pressure decreases. – Baroreflex is a short-term response to sudden changes in blood pressure. If hypertension or hypotension persists for a long period of time, baroreceptors will reset to the “new normal”, and
baroreflex mechanism will maintain hypertension or hypotension instead of normal blood pressure. – The aortic and carotid bodies also contain chemoreceptors, which detect changes in blood oxygen, carbon dioxide, and pH. The information is transmitted via the same nerves as the baroreceptors. Chemoreceptor’s primary function is to adjust respiratory volume, but reduced blood oxygen also induces sympathetic vasoconstriction, raising blood pressure. There are also central chemoreceptors located in the brainstem; they act directly on the cardiovascular center. – The cardiovascular center also receives inputs from other brain centers, and from proprioceptors in muscles and joints. This is how strong emotions
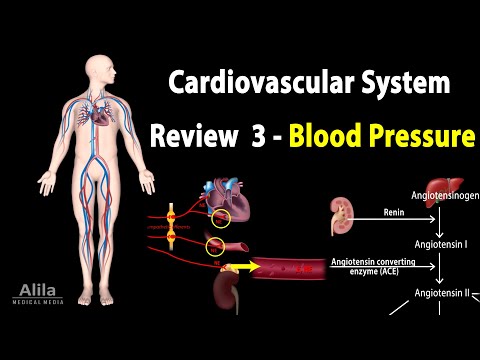
and exercise increase heart rate and blood pressure. ——————————————— – The renin–angiotensin–aldosterone system, RAAS, is a major hormonal system that increases systemic blood pressure. Renin is released from the kidneys upon a drop in blood pressure. Renin converts angiotensinogen into angiotensin I, which is then converted into angiotensin II. Angiotensin II increases blood volume and pressure via many mechanisms: it promotes sodium and water retention in the kidneys; it stimulates vasoconstriction; it induces the release of aldosterone and antidiuretic hormone – 2 other hormones that promote sodium and water retention. – Antidiuretic hormone (ADH) is a neurohormone produced in the
hypothalamus and released from posterior pituitary in response to angiotensin II and a number of other signals. Its major function is to retain water in the collecting ducts of the kidneys. At high concentrations, ADH also acts as a vasoconstrictor. – Atrial natriuretic peptide (ANP) is produced by atrial myocytes in response to chamber distension (hypervolemia). ANP promotes vasodilation, sodium and water excretion, and antagonizes RAAS, and thus reducing blood volume and pressure. – Epinephrine and norepinephrine are hormones produced by the adrenal gland upon sympathetic activation. Unlike the norepinephrine released as neurotransmitter, these are hormones carried by the bloodstream
so they have widespread impacts and longer-term effects. By binding to different receptors, they cause vasoconstriction in most organs but vasodilation in the heart and skeletal muscles, and thus directing blood flow to the heart and muscles during exercise. —————————————– – Local regulation, or autoregulation, is the ability of some critical organs to maintain constant blood flow, hence perfusion, despite changes in systemic arterial pressure. – For example, when arterial pressure decreases, baroreflex constricts much of the systemic vasculature, but blood flow to the brain remains largely unaffected. This is because the initial decrease in flow will cause small arteries
and arterioles in the brain to dilate, quickly returning the flow to normal. – Autoregulation is based on: the ability of vascular smooth muscle in small arteries to constrict or dilate in direct response to changes in blood pressure; the ability of tissues with high metabolic rates to release vasodilators, increasing blood flow; and the ability of endothelial cells to release vasoactive factors in response to changes in flow velocity or shear stress. – In the long term, a hypoxic tissue can grow new blood vessels to increase perfusion.
